The purpose of regulations and best practices for Sterilization/Decontamination is to create operating procedures that ensure safety of the staff and the medical device. Regulatory bodies stipulate standards on personal protective gear (gloves and face masks), work environment, sterilization equipment utilization and maintenance (Autoclaves, Dry ovens and Gamma ray Irradiators) and much more. One of the more critical and prominent standard setting organizations for the medical device industry is ISO.
ISO stands for “International Organization for Standardization” and is the world’s largest developer and publisher of International Standards. Numerous ISO standards provide the guidelines for the various processes within the medical device industry. Of these, the major standard that all medical device companies must be familiar with and adhere to is ISO 13485.
ISO 13485, Medical devices – Quality management systems – Requirements for regulatory purposes, is based on quality management system requirements currently contained in medical device regulations around the world, as well as those appropriate requirements contained in ISO 9001:2000. It covers the quality management requirements for organizations involved in design and development, production, installation and servicing of medical devices and the design, development and provision of related services. While ISO 13485 is a stand-alone standard, it is based on ISO 9001.
A bioburden test is an important part of the medical device sterilization process and adheres to international standards and regulatory requirements for market approval and patient safety.
Bioburden testing is a laboratory procedure that measures the number of viable microorganisms on the device’s surface to provide a baseline microbial count before the device undergoes sterilization. This is necessary to ensure the sterilization method effectively reduces the microbial load to safe levels.

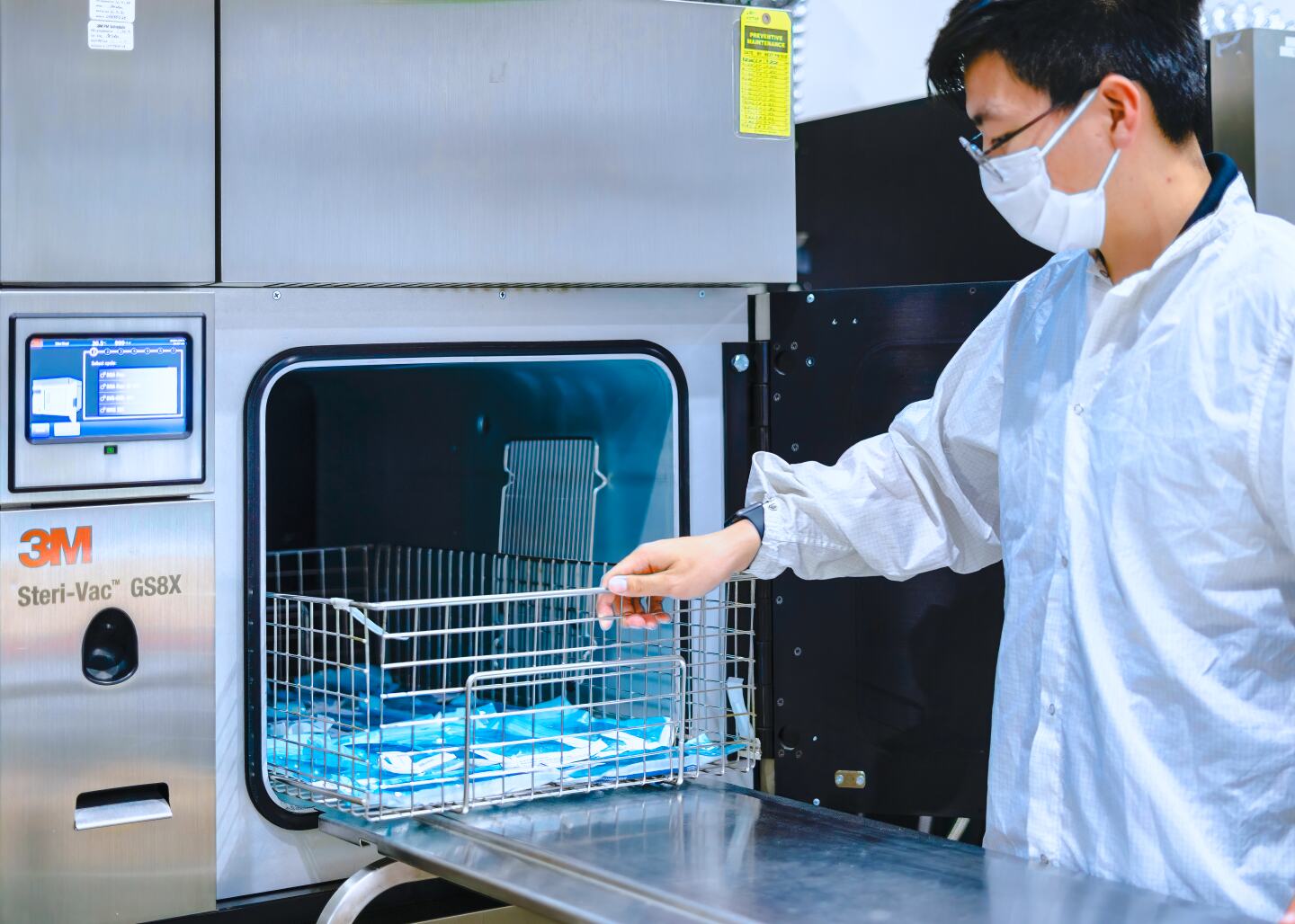
Medical device manufacturers use bioburden testing to confirm that their products are safe for use and meet regulatory standards. Sterilization service providers also use bioburden testing to help set sterilization parameters.
Bioburden testing requires aseptic techniques, controls, conducting replicates, and validation. Seven primary steps exist for performing bioburden testing:
Sample collection
Representative samples of the medical device must be tested. The sample size should reflect the typical manufacturing process and potential contamination risks.
Preparation
The test must be performed in a controlled environment to prevent external contamination. For devices with complex geometries or surfaces, rinsing or swabbing methods may be used to collect microorganisms.
Extraction
There are two microorganism collection methods: Rinsing method and swabbing method.
Microbial enumeration steps
Filtration: The extraction fluid is passed through a membrane filter that traps microorganisms.
Plating: The membrane filter or aliquots of the extraction fluid are plated onto nutrient agar plates.
Incubation: The agar plates are incubated under temperature and duration conditions suitable for microorganism growth.
Counting colonies
After incubation, the number of colonies on the agar plates are counted.
Calculation
Dilution factors, extraction fluid volume, and the area of the device sampled are used to calculate the total bioburden.
Documentation and reporting
Test data is recorded, results are analyzed to determine if bioburden levels are within acceptable limits, and a detailed report is prepared documenting the procedure, results, and conclusions. The report is necessary for regulatory submissions and quality assurance.

Medical device bioburden testing is required to meet regulations in the United States. Medical device manufacturers must perform bioburden testing as part of the process validation for sterilization methods and is outlined in several FDA guidelines and standards, including ISO 11737-1.
Receive the latest infographics, guides, and blog updates for medical device manufacturing, package testing, and sterilization.